Antenatal admission - This
page has been designed to be used in women presenting
to labour ward or
assessment area not in established labour e.g.
diminished fetal movements, PV bleeding. Prompts
to support
history taking have been included. Space to document
clinical findings: - maternal observations, fetal
heart assessment, contractions. Free text is
included on the reverse of this page. |
Antenatal Admission
|
There is space at the bottom of the page to record
number of admissions.
If inpatient antenatal care
is required the page can be used as the admission
and further free text written on history sheets. |
| |
|
|
|
|
|
Page 1 - Lists personal
details and identifies lead care
providers during labour. A section is included
for recording signatures of everyone who writes
in the notes.
|
| |
|
|
|
Page 2 - Pregnancy assessments -
space to document information on medical, social
and previous obstetric history with prompts included
for salient points. Risk factors identified
from the assessments are recorded in the relevant
boxes at the top of pages two and nineteen, ensuring
that any identified risks can be highlighted throughout
the intrapartum period. Space to record
and review maternal preferences is also provided.
|
|
Page 3 - Initial assessment - presenting
history includes prompts to support history taking.
Space to document clinical findings for: maternal
observations, fetal heart assessment, contractions
and vaginal assessment.
Additional pages are available
if required
|
| |
|
|
Page 3a/b -
Induction of labour |
|
Page 3a/b - Induction of Labour -
is documented on a separate sheet, which is secured
into the notes by an adhesive strip. There is space
to record reason for induction as well as maternal
observations, cervical assessment and action taken.
Additional sheets are available if required. |
| |
|
|
|
Pages 4 – Management plan – an agreed plan
of care for labour and delivery can be recorded
here, and updated or amended as the labour progresses.
Space to record if the pregnancy notes have been
reviewed at the beginning of labour is situated
on this page.
|
|
Pages 5 - Free text pages, for all professionals providing
care to document chronologically the progress
during labour. Vaginal examination stickers
are provided, to be used as indicated.
|
| |
|
|
|
Page 6 - Free text pages, for all professionals providing
care to document chronologically the progress
during labour. Vaginal examination stickers
are provided, to be used as indicated.
|
|
Page 7 -Free
text pages, for all professionals providing
care to document chronologically the progress
during labour. Vaginal examination stickers
are provided, to be used as indicated.
|
|
|
|
|
Page 8 -Free
text pages, for all professionals providing
care to document chronologically the
progress during labour. Vaginal examination stickers
are provided, to be used as indicated.
|
Pages
8 & 9
|
Page 9 -Free
text pages, for all professionals providing
care to document chronologically the
progress during labour. Vaginal examination stickers
are provided, to be used as indicated.
|
|
|
|
|
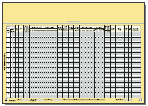
Pages 10 & 11 – Partogram - the layout is
in A3 format. The layout allows clinical findings
to be recorded left to right, in quarter hourly
intervals. They include: maternal observations,
fetal heart rate, contractions, fluids and drugs.
Within the cervicogram, dilatation and
descent have been documented separately, starting
from left and right, respectively. As labour
progresses, cervical dilatation increases and
descent of the head occurs, the plotted lines
move towards each other and eventually meet.
|
Pages
10 & 11
|
Included in the partogram are prompts
for time of rupture of membranes and onset of
second stage, to facilitate concise documentation. Also
included is a recommendation for
the maximum number of contractions when using
oxytocin.
Additional pages are available
if required.
|
| |
|
|
|
Page 12 - Free text page, for
all professionals providing care, to document
events chronologically. As with the previous
free text pages, vaginal examination stickers
are available for inclusion here. Additional
pages are available if required.
|
|
Page 13 -Free text page, for
all professionals providing care, to document
events chronologically. As with the previous
free text pages, vaginal examination stickers
are available for inclusion here. Additional
pages are available if required.
|
| |
|
|
|
Page 14 - Free text page, for
all professionals providing care, to document
events chronologically. As with the previous
free text pages, vaginal examination stickers
are available for inclusion here. Additional
pages are available if required.
|
Pages
14 & 15
|
Page 15 – Procedures -
Space to document clearly; discussion of risk and
benefit to be undertaken about clinical procedures
i.e. third stage management, epidurals etc. |
| |
|
|
Page 16 and Page 17
-
Operative delivery |
|
Pages 16 & 17- Should
an operative procedure be indicated, space
has been included to document all aspects, not only
the clinical procedure but also: personnel present,
timings of procedure and post-operative instructions.
This page can be used to document assisted deliveries,
caesarean sections, manual removal of placenta or
suturing of a 3rd or 4th degree
tear. |
| |
|
|
| Page 18 - Post delivery - Space
to document clinical findings regarding third
stage management, assessment and repair of the perineum, and
immediate postnatal observations. |
|
Page 19 - Mother’s birth
summary -
space to document all aspects pertaining to delivery,
including type of delivery and timing of stages of
labour. There is also a prompt to document any postnatal risk
factors identified. |
| |
|
|
| Page 20 - Baby’s birth summary - Space
to document information about the birth pertaining
to the baby such as: Apgar scores, resuscitation,
initial examination and feeding. There is also a
prompt to document any further risk factors. |
|
|